In under a year, Gary and Arianna Lafreniere, owners of A Place At Home – Merrimack Valley, have provided over 7,000 hours of care to the families in the community and surrounding areas of Chelmsford, Massachusetts.
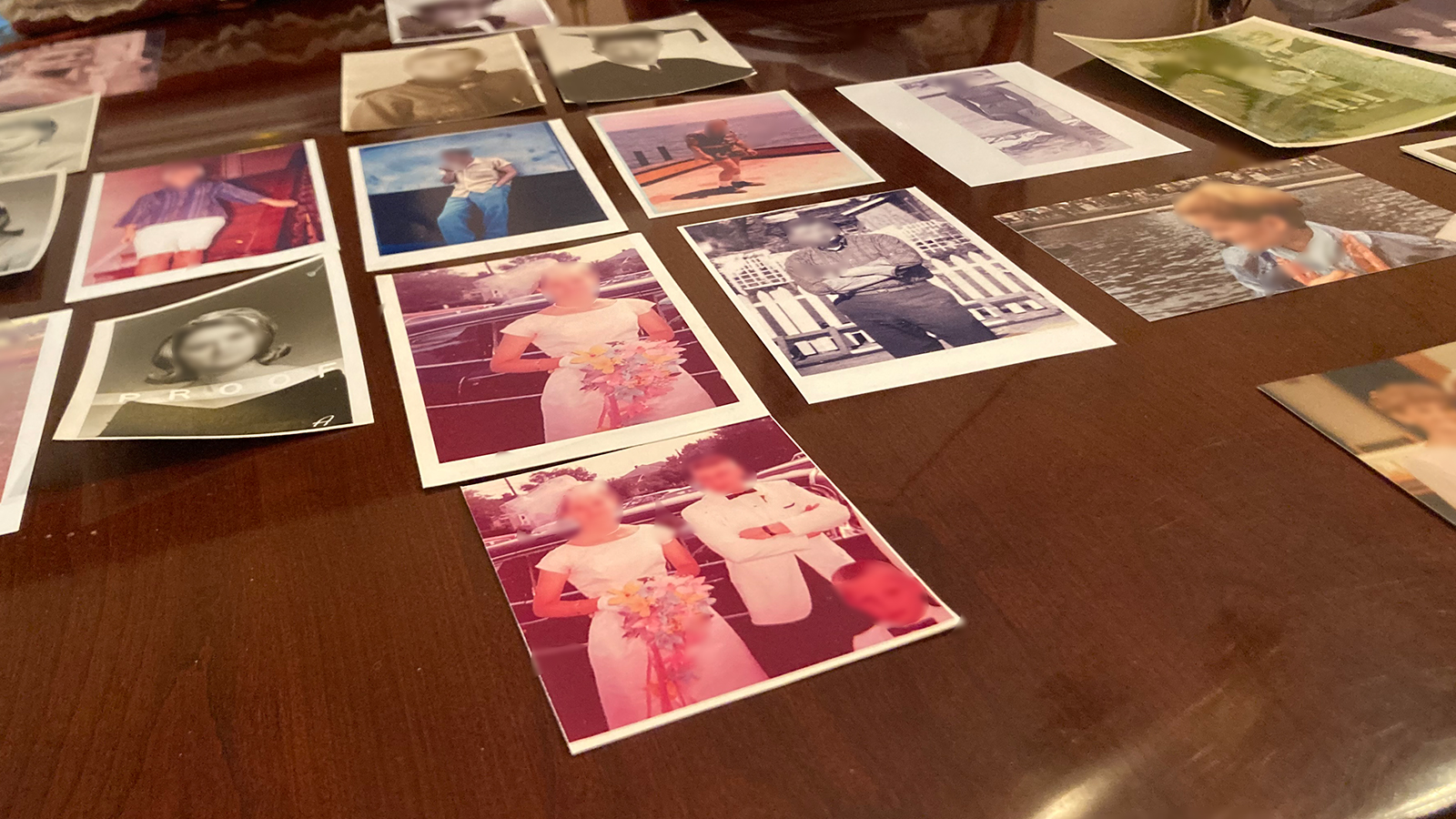
It’s a great start to their mission of helping people stay safe and healthy as they navigate the aging process. They opened their doors in February of 2021. The inspiration behind starting an in-home care agency is Gary’s mom. She was diagnosed with dementia in 2016. Gary and Arianna were both working full time and raising three young children. Gary remembers when the phone calls with his mom started becoming odd. She would request the same things over and over. When it first started, Gary and Arianna assumed she was becoming forgetful as she aged. They had no knowledge of dementia or what the signs were.
Gary says the day he knew it was something more was when she asked him when his birthday was.
The birthday conversation was the catalyst for a doctor’s appointment that eventually led to a dementia diagnosis. Shortly after that diagnosis, Gary’s mom suffered a fall. Fortunately, she was unharmed, except for a bump on her head. But she didn’t remember the fall at all. Gary clearly remembers thinking at the time how much he’d wished he’d known about the signs and symptoms of dementia before it had become so progressed in his mom. At that point, they knew it wasn’t safe for her to remain in her home. His mom lived by herself, and the family saw her often, but they couldn’t be with her all the time. They moved her into an assisted living community, and eventually, she was moved into Memory Care within the same building.
At the time, Gary and Arianna didn’t know what to do beyond that.
Gary shares, “Our knowledge of what could be done is that we’d have to hire a nurse, and we couldn’t afford that, knowing what a nurse would cost.” Back then, the couple wasn’t aware of in-home care as an option. Arianna says that if they’d known, that’s the route they would have started with. Having a caregiver in the home with Gary’s mom when they couldn’t be there would have provided safety and peace of mind. Fortunately, their experience was not a terrible one. Gary’s mom was safe and comfortable in the senior living community, and the staff that cared for her were genuinely invested in her happiness and quality of life.
“They treated her like she was their mother, and we really began to understand their job and gained an appreciation for caregivers from that perspective.”

The experience with his mom was still on their minds later when the couple began considering what they wanted to do next, professionally. They knew they wanted it to be less about the money and more about helping people. They wanted something rewarding that would allow them to lay their heads on their pillows at night and feel good about their day. Gary says that opening an in-home care agency for seniors was the obvious choice. Arianna agrees, recalling the stress they felt when navigating the situation with her mother-in-law and the energy they’d put toward educating themselves and learning more about the disease.
“You’re kind of left to your own devices. You can research and find resources, but we really didn’t even know that in-home care existed for something like what mom had. So discovering that option really spoke to us.”
The couple decided to open A Place At Home – Merrimack Valley, and it couldn’t have come at a better time for the community. The COVID-19 pandemic was in full force. What might have been a daunting idea – opening a new business while businesses everywhere were struggling heavily or closing their doors altogether – ended up being a key reason that the Lafrenieres decided to move forward. Gary says they saw the need for home care in their community. Families who had been preparing for their loved ones to move into assisted living found themselves having to pivot and come up with other solutions that kept their parents and grandparents safer during the pandemic. Gary says they didn’t second guess their decision to open when they did.
“People were bringing their parents home, so they needed us. We never looked at it like, oh, this is bad timing. We just knew we had some challenges we would have to work around.”
Arianna recalls the research they did so they’d know what was needed for them and their caregivers to go into homes safely. They poured their energy into discussions with A Place At Home headquarters, understanding how other locations were handling the pandemic, ensuring they had proper PPE and safety protocols so that the clients and the families they served could be confident in the care of their loved ones. The public health emergency reinforced their desire to open their doors. “It was even more important for us to be up and running and available for those that wanted to bring them home.”
The experience with Gary’s mom left the couple with a desire to advocate for seniors with dementia and their families. In October, A Place At Home- Merrimack Valley were sponsors of the Alzheimer’s Walk. Money raised during the event goes toward further research of the disease that 55 million people live with worldwide. That day, the Alzheimer’s Walk raised half a million dollars. Gary says, “We’ll continue to be there every year, without a doubt. We were proud to be a part of that.”

Now, Gary and Arianna advocate for seniors and their families on a daily basis.
Gary says the word they repeatedly hear when they meet with families is “overwhelmed.” Arianna remembers the sense of being overwhelmed herself as she made the initial phone calls, trying to figure out what to do and how to navigate the situation with her mother-in-law. But, she says now, owning an in-home care business, their experience has set them apart. They’ve been able to help and coach the families they come in contact with.
Gary agrees, sharing that more than anything, their experience with his mom inspired them to help people navigate the waters of “what do I do?”. Even if his mom had been able to stay in her home longer, eventually, she would have had to transition to Memory Care as her disease progressed. So now, when Gary and Arianna meet with families who are going through similar experiences, the couple’s focus is on listening to what the situation is, learning about what the family and their loved one’s needs are, and then offering advice and guidance that will best serve the senior’s health and quality of life. Often, that means providing care in their home. But, sometimes, that’s not a safe or sustainable option. In that case, the Lafrenieres help families navigate the process of finding an assisted living or memory care community that is better suited for their needs.
“That’s where we like to start, to ease that pain of being overwhelmed and give them the comfort of knowing that it’s something we can help with. It’s not something that we just researched. We lived it.”
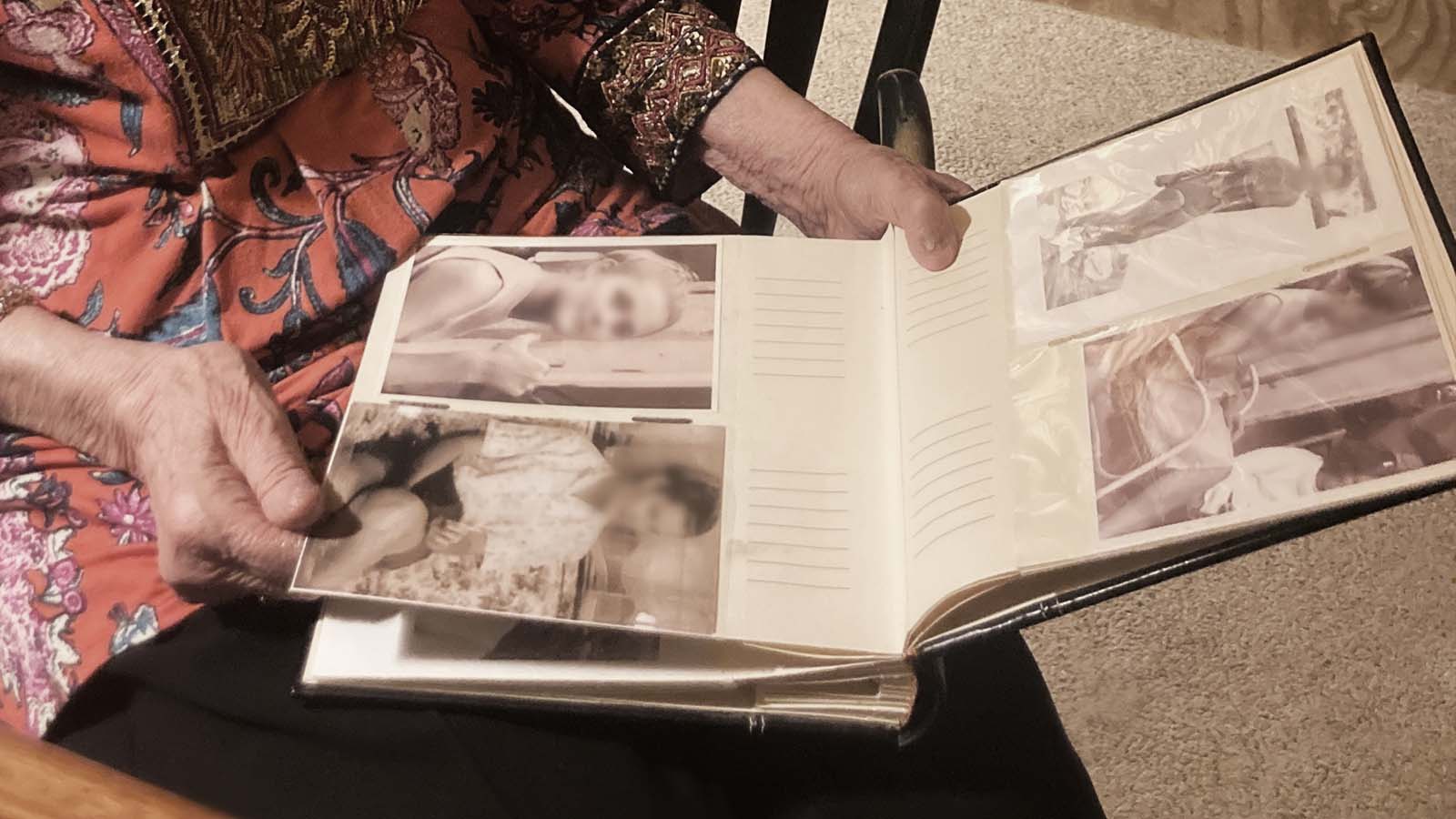
Less than a year in, the couple is already impacting families in Chelmsford in a significant way. One of their clients is a couple who just celebrated their wedding anniversary. The family began to notice that their mom was struggling to care for herself. Their dad was in good health and helped as much as he could, but the family was at a point where they were considering their options. They either had to move their mom into an assisted living community – separating the couple – or they had to hire someone to come in for extra support.
Together, the family opted to bring care into the home, choosing A Place At Home – Merrimack Valley as their care provider. The decision has been a good one. The couple has grown close to their caregiver, and they recently spent time with their family and friends celebrating their anniversary in a way they wouldn’t have been able to if one of them was living in assisted living.
The effect in their community hasn’t just been with seniors and their families.
Gary and Arianna have profoundly rooted respect for caregivers. After seeing the compassionate way his mother was cared for, the couple is clear about where their priorities lie. Clients are their top concern – right along with their caregivers. Gary shares about their caregivers, “Their lives, their happiness, their jobs – are as much of a priority as the service our clients get.” And it’s not lip service. Gary and Arianna worked with a CNA school in their state to secure scholarships for caregivers that want to advance their careers.
The first caregiver to be awarded a scholarship is almost finished with the course.
When she applied to work with Gary and Arianna, she didn’t have any professional caregiving experience on her resume. She had, however, been a family caregiver for her grandmother. Recalling how the caregivers had treated Gary’s mom like their own, they knew she would be a good fit. At first, Gary and Arianna scheduled her with clients that needed a lower level of care. As her employment progressed, they put her through CareAcademy training to enhance her skill set. She caught on quickly, and because the Lafrenieres believe in investing in their employees, she’s on her way to being a Certified Nursing Assistant, advancing her career in the healthcare industry.
Gary and Arianna are happy to be able to offer support within their community. Chelmsford is where Gary grew up; Arianna grew up in a town 20 minutes north of there, and it’s where they’re raising their family. The couple is grateful to help the seniors and families that need extra support and invest in the futures and ambitions of their employees.
“It’s not just caring for the individuals that need this; it’s about the families in general. Knowing what we went through – the rewarding part is getting to allow someone to stay at home a little bit longer and stay comfortable and happy in their home, but you’re also helping the entire family.”
If you or a loved one are in the Merrimack Valley area and are overwhelmed and in need of support and care, you can find more information about the Lafrenieres and how they can help here.