If you or a loved one has received a dementia diagnosis, understanding the 7 stages of dementia in seniors can help you prepare for what’s ahead. Dementia progresses through different stages, and knowing what to expect at each one allows families to provide the right care and support along the way.
According to the Alzheimer’s Association, over 7 million Americans age 65 and older are living with dementia, and that number is expected to grow as the population ages. In this article, we’ll explain what dementia is, explore the factors that cause it to progress, outline the seven stages of dementia, offer guidance on caring for your loved one through each stage, and discuss when it may be time to seek professional help.
What Is Dementia and How Does it Affect Seniors?
Dementia is a progressive condition that causes a loss of cognitive functions such as thinking, remembering, and reasoning. These changes interfere with daily life and can affect a senior’s ability to live independently. According to the World Health Organization (WHO), 57 million people worldwide had dementia in 2021. With the increasing prevalence of dementia in seniors, it is essential to understand the different kinds of dementia and their stages.
Common types of dementia include:
- Alzheimer’s disease: Caused by changes in the brain, it is the most common form of dementia.
- Frontotemporal dementia: A rare type that primarily affects individuals under the age of 60.
- Lewy body dementia: Linked to abnormal deposits of a protein called alpha-synuclein in the brain.
- Vascular dementia: Results from reduced blood flow or damage to blood vessels in the brain.
- Mixed dementia: Occurs when two or more types of dementia are present simultaneously.
What Causes Dementia to Progress Through Its 7 Stages?
Dementia worsens over time due to ongoing damage to brain cells. In conditions like Alzheimer’s disease, abnormal protein buildup disrupts communication between nerve cells, eventually leading to cell death.
Other factors influencing progression include:
- Genetics: A family history of dementia can increase susceptibility to certain types of dementia.
- Overall health: Conditions such as diabetes, high blood pressure, and heart disease can reduce blood flow to the brain and accelerate cognitive decline.
- Lifestyle factors: Poor nutrition, lack of physical activity, smoking, or excessive alcohol use may worsen symptoms over time. According to the CDC, nearly 1 in 4 adults over 65 experience a fall each year, and poor cardiovascular health can accelerate cognitive decline.
- Emotional and social well-being: Isolation, chronic stress, and untreated depression can negatively affect brain health and cognitive function.
Early diagnosis, proper medical care, and a healthy lifestyle can slow symptom progression and improve quality of life.
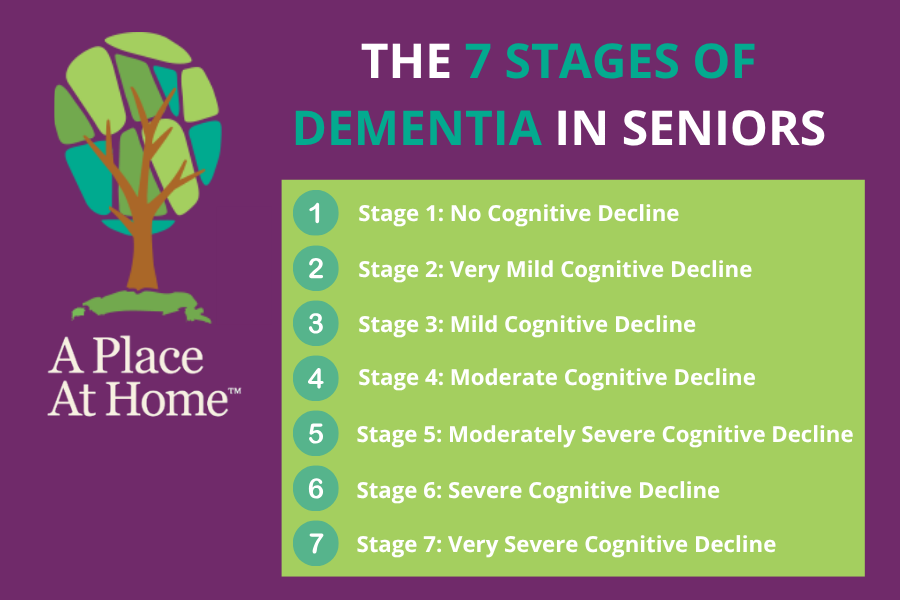
The 7 Stages of Dementia in Seniors
It’s essential to understand the various stages of dementia, including their symptoms, typical duration, and recommended caregiving strategies, so you can provide the best possible care for your loved one.
Stage 1: No Cognitive Decline
At this stage, dementia has no noticeable impact on daily life, and your loved one continues to function normally. However, if you suspect early signs of dementia, it’s wise to begin planning together. Take time to discuss your loved one’s values, preferences, and priorities for future care so you’ll be prepared as symptoms progress.
Stage 2: Very Mild Cognitive Decline
In this stage, you may begin to notice mild forgetfulness, though these changes might not be evident to medical professionals. Daily memory lapses may appear similar to those associated with normal aging. Your loved one might have trouble finding the right words or occasionally substitute one word for another, but they are generally able to function normally at work, at home, and in the community.
As with stage 1, it’s important to start planning for the later stages of dementia to ensure your loved one receives the care they will eventually need. Pay close attention to any new symptoms, as early recognition can help with timely support and intervention.
Stage 3: Mild Cognitive Decline
At this stage, dementia has minimal impact on your loved one’s overall quality of life, though you may notice subtle changes in thinking and reasoning. Memory loss may become more apparent, such as misplacing items and struggling to retrace steps to find them. They may also have difficulty remembering appointments, managing finances or medications, paying attention, or performing well at work.
It’s important to start planning for the future, as dementia will eventually progress. Consider creating a document that outlines your loved one’s values and priorities for each stage of the disease, ensuring their preferences guide care decisions.
Building a trusted healthcare team is also essential, one that will honor your loved one’s wishes. You may need to provide support with tasks such as scheduling appointments, managing bills and medications, organizing legal and financial documents, and assisting with driving if necessary. Early planning helps maintain independence and ensures your loved one receives care that reflects their needs and values.
Stage 4: Moderate Cognitive Decline
At this stage, your loved one can still remember their past and recognize family and friends. However, they may struggle with familiar words and have difficulty completing daily tasks such as cooking, laundry, and shopping. Unfamiliar places can feel overwhelming, and managing finances may become challenging.
You can support them by planning for the later stages of dementia. Consider creating a document that outlines their values and priorities for each stage, ensuring their wishes guide future care. You may also need to assist with everyday tasks, take over driving, and provide hands-on support to help them maintain safety and comfort.

Stage 5: Moderately Severe Cognitive Decline
At this stage, your loved one may still remember their past and recognize family and friends, but they will have difficulty making healthcare decisions on their own. They will require support at home for everyday activities and may experience personality changes, mood swings, repeated questions, memory gaps, and confusion about dates, locations, or personal information like their address and phone number. They may also need help with eating, toileting, choosing season-appropriate clothing, and managing bladder issues.
It’s important to create a document outlining their care preferences and to communicate these with their healthcare team, ensuring that all care decisions respect their wishes. Daily support will likely include assistance with dressing, toileting, and other routine activities. Responding to repeated questions with patience and understanding can help reduce frustration and maintain their dignity.
Stage 6: Severe Cognitive Decline
At this stage, your loved one may lose awareness of their surroundings and exhibit significant personality changes. They may have little or no memory of their past and may not recognize family and friends. Making healthcare decisions will likely be difficult, and they may require 24-hour support for daily activities.
Major mood swings and personality shifts are common. They may also experience delusions, such as insisting they need to go to work despite no longer being employed. Assistance with toileting, dressing, and daily routines will be necessary, and they may become disoriented or wander.
Supporting your loved one involves helping with basic daily activities while finding ways to connect beyond conversation. Activities such as listening to music, reading aloud, or looking through photo albums can provide comfort and meaningful engagement.
Stage 7: Very Severe Cognitive Decline
At this stage, your loved one may lose the ability to respond to their environment and will require full-time care. This is considered the end stage of dementia, where all previous stages have progressed, and they are no longer able to perform self-care.
Over time, they may lose the ability to communicate their needs and may also lose physical functions, such as walking, as they may no longer remember how. Full assistance will be needed for all daily activities, including bathing, dressing, eating, toileting, and other basic needs. Depending on their age and overall health, this final stage typically lasts around 1–2 years.
How to Care for a Loved One Through the 7 Stages of Dementia
Every stage of dementia brings unique challenges for both the individual and their family and friends. Having a care plan in place for each stage helps ensure that your loved one’s needs are met with compassion, consistency, and respect.
- Early Stages: Encourage independence and establish routines. Gentle reminders and structured activities can help maintain confidence.
- Middle Stages: Implement safety measures, simplify tasks, and provide supervision. Labeling items, organizing medications, and breaking tasks into steps can reduce frustration.
- Late Stages: Focus on comfort, dignity, and advanced care needs. Provide emotional reassurance, assist with all personal care, and work closely with healthcare professionals.
When to Seek Professional Help for Dementia Care
If you notice that your loved one is experiencing significant memory loss or struggling with daily activities such as bathing, toileting, doing laundry, or managing household chores, or if you have concerns about their safety or ability to care for themselves, it’s important to take action. Speak with their healthcare professional as soon as possible. They can assess your loved one’s needs and help determine the most appropriate care options, whether that’s in-home dementia care, assisted living, a memory care community, or a nursing home.

Dementia Home Care Services in Palmetto, FL
Caring for a loved one with dementia can be emotionally and physically demanding, especially as the disease progresses through its various stages. Having professional support can make all the difference, both for your loved one’s well-being and your own peace of mind.
At A Place At Home – Palmetto, we specialize in compassionate, personalized dementia in-home care designed to help seniors live safely and comfortably in familiar surroundings. Our trained caregivers assist with daily activities, medication reminders, companionship, and emotional support while preserving your loved one’s dignity and independence.
We understand that every person’s journey with dementia is unique. That’s why our care plans are tailored to meet your loved one’s evolving needs, from early-stage support to full-time assistance in later stages. Our goal is to give families the confidence that their loved one is receiving the highest quality of care.
If your loved one has been diagnosed with dementia or is showing signs of cognitive decline, A Place At Home – Palmetto is here to help. Call us today at (941) 541-2311 to schedule a free consultation and learn more about our dementia home care services. Together, we can create a care plan that ensures safety, comfort, and dignity at every stage of the journey.
Frequently Asked Questions (FAQs)
How fast does dementia progress?
Dementia typically progresses over several years, though the rate varies by individual and type. Alzheimer’s disease, for example, often advances through all seven stages over 8–10 years. Lifestyle, genetics, and medical treatment can slow or accelerate the rate of decline.
What is the life expectancy of a person with dementia at 75?
The average life expectancy of a 75-year-old with dementia ranges from 4 to 8 years after diagnosis, depending on overall health, type of dementia, and quality of care. Some people live longer, especially with early intervention, medical management, and strong caregiver support.
How can you tell what stage of dementia a person is in?
You can tell what stage of dementia a person is in by observing changes in memory, communication, daily function, and behavior. Early stages involve mild forgetfulness, while later stages include confusion, disorientation, and loss of independence. A healthcare professional can assess symptoms to determine the exact stage.