Watching an elderly parent wake up multiple times during the night can be exhausting and worrying. Sleep is essential for memory, mood, immunity, heart health, balance, and overall well‑being. Many families assume sleep problems are simply part of aging, but frequent nighttime awakenings are often a sign of underlying issues that can be addressed.
How Common Are Sleep Problems Among Seniors in Florida
According to the U.S. Department of Health and Human Services data from the 2022 Behavioral Risk Factor Surveillance System, about 27.9 percent of adults age 65 and older in Florida report sleeping less than seven hours per night, which is below the recommended amount for healthy adults. This shows that insufficient sleep is a significant concern for older Floridians.
Pembroke Pines specifically has a growing senior population, with about 19.5 percent of residents aged 65 and over, which is higher than the national average. This makes sleep issues particularly relevant to families in the area.
Nationwide data also indicate that nearly half of older adults experience insomnia or poor sleep quality, with many seniors unaware that their sleep challenges could be addressed with proper support. Sleep disruptions are not just inconvenient; they can have real health consequences.
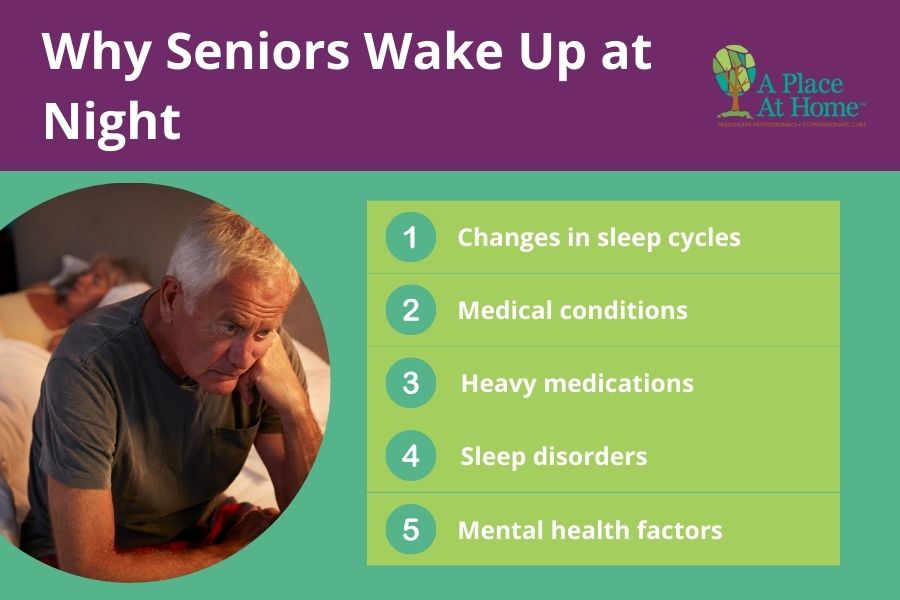
Why Seniors Wake Up at Night
There are several factors that contribute to frequent nighttime waking in older adults, often interacting with one another:
- Changes in sleep cycles: Seniors often experience lighter sleep and earlier waking times.
- Medical conditions: Pain from arthritis, heart or lung problems, diabetes, or bladder issues can interrupt sleep.
- Medications: Drugs for blood pressure, mood, or pain may cause insomnia or fragmented sleep.
- Sleep disorders: Sleep apnea, restless leg syndrome, and insomnia are more common in older adults. Studies suggest that 20 to 60 percent of people over age 65 show signs of sleep apnea.
- Mental health factors: Anxiety, depression, or cognitive changes can affect the ability to stay asleep.
The Consequences of Poor Sleep
Sleep is not simply rest. It is the period when the body repairs tissues, strengthens the immune system, consolidates memories, and regulates hormones. When seniors do not sleep well, the effects extend beyond fatigue. Cognitive performance may decline, memory lapses can increase, and the ability to focus and make decisions diminishes. Physical health is also affected. Poor sleep is associated with a higher risk of falls, slower healing, and worsening chronic conditions such as diabetes and heart disease.
The impact extends to family caregivers as well. Nighttime caregiving, especially when parents wake up multiple times, can lead to exhaustion, stress, and burnout. Families may find themselves navigating work, daily responsibilities, and caregiving all at once, often without the support needed to manage these demands. Improving sleep is essential not just for seniors but for the well-being of the entire household.
Practical Strategies to Support Better Sleep in Seniors
Addressing sleep challenges usually requires a combination of lifestyle changes, environmental adjustments, and medical support. The following strategies are recommended by geriatric care experts:
- Create a consistent sleep schedule. Seniors benefit from going to bed and waking at the same time every day. A calming pre-bedtime routine, such as reading, listening to soft music, or gentle stretching, helps signal to the brain that it is time to sleep.
- Optimize the bedroom environment. A cool, dark, and quiet room promotes restorative sleep. Comfortable bedding and supportive mattresses improve physical comfort. Limiting bright screens in the evening helps the body naturally prepare for sleep.
- Monitor diet and hydration. Avoiding caffeine and large meals in the evening can prevent sleep disruption. Encouraging fluids earlier in the day reduces nighttime trips to the bathroom while maintaining proper hydration.
- Encourage daytime physical activity and natural light exposure. Gentle exercises such as walking or stretching support deeper sleep at night, while exposure to daylight during the day helps regulate circadian rhythms.
- Consult a healthcare provider. If medications or health conditions are contributing to nighttime awakenings, a doctor can review treatment plans. Evaluations for sleep disorders such as sleep apnea or restless leg syndrome can help identify underlying causes.
- Keep a sleep diary. Recording bedtime, wake times, nighttime awakenings, medication schedules, and daily fatigue can provide valuable insight for healthcare professionals in tailoring solutions.
Overnight Care Support in Pembroke Pines, Florida
Sometimes seniors need support beyond routine changes and lifestyle adjustments. A Place at Home‑Weston provides compassionate overnight care in Pembroke Pines, Florida, offering:
- Assistance with bedtime routines and mobility
- Medication reminders and bathroom support
- Gentle companionship throughout the night
- Supervision to reduce nighttime anxiety and falls
Overnight care allows seniors to rest more comfortably and gives families confidence that their loved ones are safe and supported.

If your parent struggles with nighttime awakenings, contact A Place at Home‑Weston to learn how our overnight care services can help improve sleep and overall well-being for your loved one. Call (954) 335-9284
FAQs Related to Sleep Issues in Seniors
Is it normal for seniors to nap during the day if they sleep poorly at night?
Short daytime naps can be helpful, but long or late-afternoon naps may make nighttime sleep more difficult. Seniors generally benefit most from brief naps earlier in the day, especially if nighttime sleep is fragmented.
What is the emotional impact of poor sleep on seniors?
Ongoing sleep disruption can affect mood, increase irritability, and contribute to feelings of isolation or frustration. Supporting better sleep often leads to noticeable improvements in emotional well-being and daily engagement.
Can nighttime waking be linked to memory loss or dementia?
Yes. According to research published in BMC Geriatrics, sleep-wake disorders, including frequent night awakenings and irregular sleep patterns, occur in most people living with dementia and are a common feature of cognitive decline, contributing to disrupted nighttime rest. In this study, researchers note that sleep-wake disorders include frequent nocturnal awakenings and poor sleep efficiency, and that these symptoms burden both the individual and caregivers.
How does poor sleep affect fall risk in older adults?
Interrupted sleep can lead to grogginess, slower reaction time, and poor balance, especially during nighttime bathroom trips. Adequate supervision, proper lighting, and assistance during the night can significantly reduce fall risk.
How does overnight care differ from having a family member “check in” at night?
Professional overnight caregivers remain alert and present throughout the night, providing consistent supervision, assistance, and reassurance. This level of support reduces risks that brief or intermittent check-ins may miss.

