When most people think of Parkinson’s disease, tremors or involuntary shaking of the hands often come to mind. But for many seniors, tremors are not the first symptom and sometimes never become the most noticeable one.
Parkinson’s often begins quietly, with subtle changes in movement, sleep, mood, digestion, or thinking that can easily be mistaken for normal aging. Understanding these early indicators matters. Earlier recognition leads to earlier support, better symptom management, and improved quality of life for seniors and their families. According to the Parkinson’s Foundation, nearly 1 million people in the United States are currently living with Parkinson’s disease, and that number is expected to rise to 1.2 million by 2030, largely due to the aging population.
Key Takeaways (Quick Summary)
- Parkinson’s often begins without tremors, especially in seniors
- Early symptoms are frequently non-motor, such as sleep changes, constipation, or mood shifts
- Symptoms usually develop gradually and progressively, not suddenly
- Changes may appear on one side of the body first
Early recognition allows for safer routines, better care planning, and greater independence
Tremors Aren’t the First Sign of Parkinson’s
Contrary to popular belief, Parkinson’s disease doesn’t always start with a noticeable tremor. In seniors, it often begins years before any shaking appears. Early signs can show up in subtle ways, slower movements, changes in handwriting, stiffness, difficulty sleeping, shifts in mood, digestive issues, or even a reduced sense of smell. Because these symptoms overlap with normal aging, they are frequently overlooked or dismissed. Recognizing these early indicators in seniors is critical, as it allows for timely evaluation, better management, and support that can make daily life safer and more comfortable.
Why Parkinson’s Is Often Missed in Seniors
Parkinson’s can be difficult to detect early, particularly in older adults. Tremors, the symptom most commonly associated with the disease, often show up later in its progression.
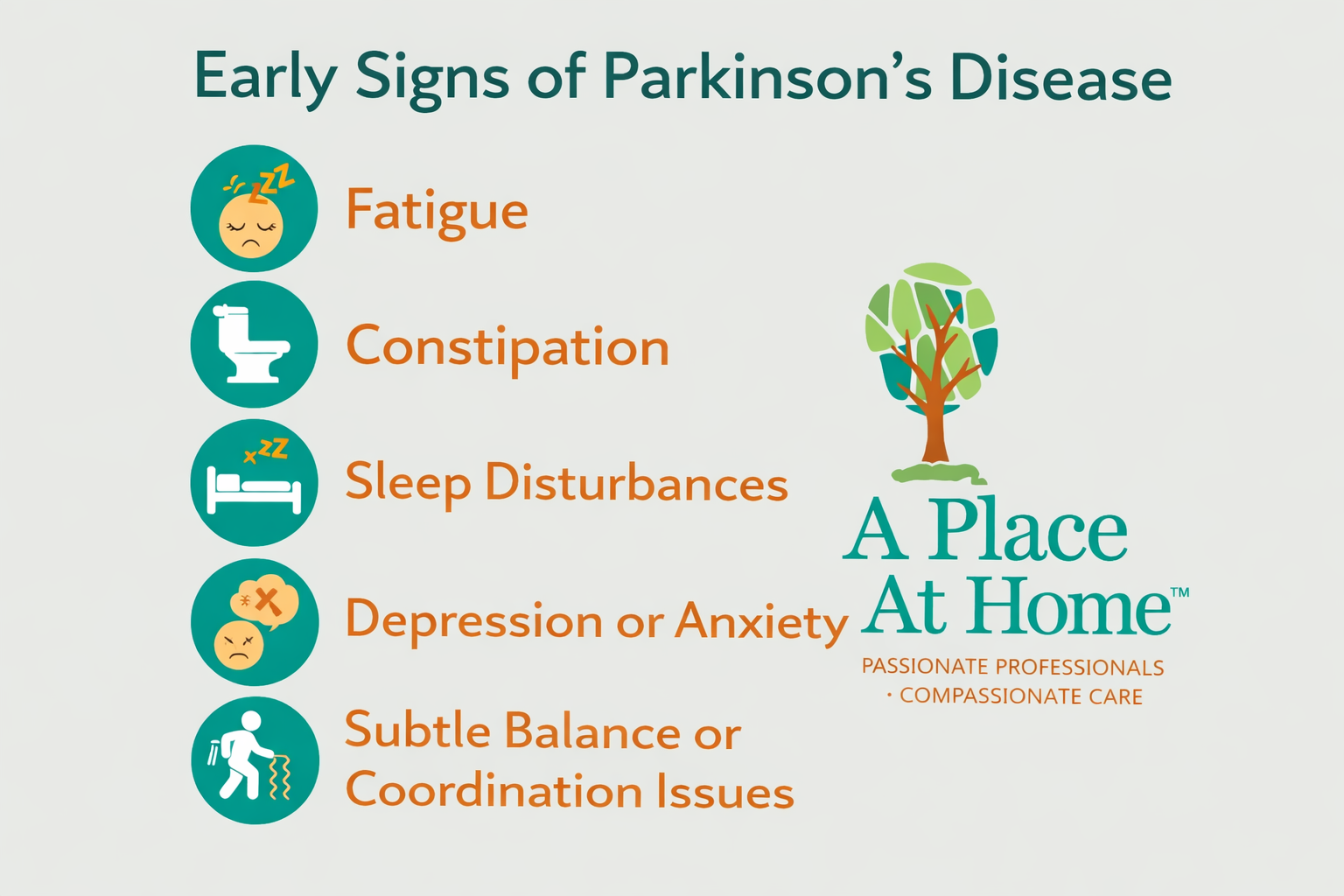
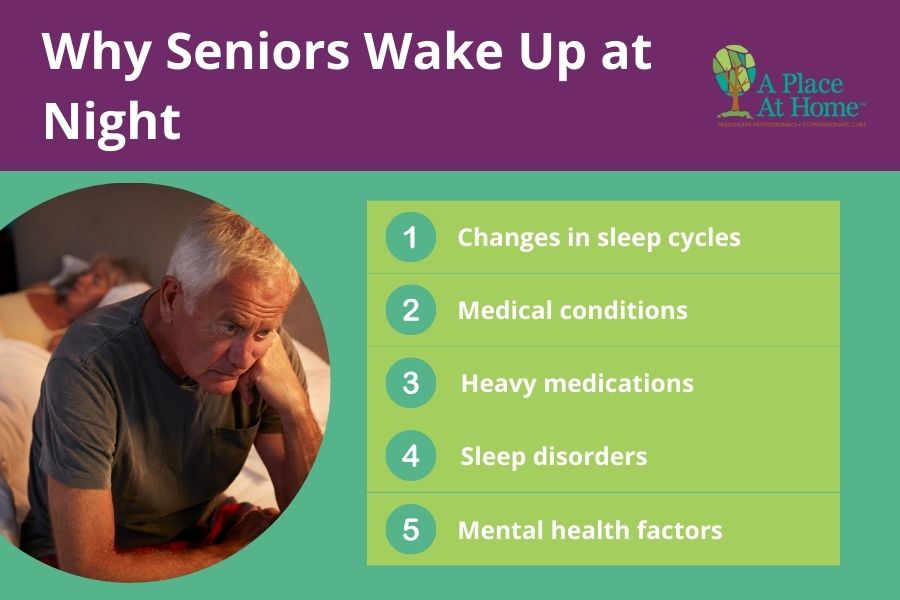
In early stages, Parkinson’s may present with:
- Fatigue
- Constipation
- Sleep disturbances
- Depression or anxiety
- Subtle balance or coordination issues
These changes are frequently attributed to aging, stress, or other chronic conditions. Even healthcare providers may not immediately connect these symptoms without a clear pattern over time.
That is why family members and caregivers play a critical role in noticing gradual changes and advocating for further evaluation when something feels “off.”
What is Parkinson’s Disease?
Parkinson’s disease is a neurodegenerative disorder, which means it gradually damages the brain over time. Specifically, it affects neurons that produce dopamine, a chemical responsible for controlling movement, coordination, and certain brain functions. Because these neurons are lost slowly, Parkinson’s develops progressively rather than suddenly.
There is no single early symptom that defines the disease, each person may notice different signs first, from subtle movement changes to shifts in mood, sleep, or daily habits. Understanding Parkinson’s as a progressive, multi-symptom condition helps seniors, families, and caregivers recognize early changes and seek support before the condition advances.
The Earliest Signs of Parkinson’s in Seniors
Recognizing the earliest symptoms of Parkinson’s in your senior loved ones can help ensure that they get the care and treatment they need right away to manage symptoms and ensure a better quality of life
Non-Motor Symptoms
While tremors often grab attention, the earliest signs of Parkinson’s in seniors are usually non-motor and they can appear years before any shaking. Being aware of these subtle changes is critical for early recognition and care.
- Loss of sense of smell: One of the first warning signs, seniors may notice foods or fragrances don’t smell as strong as they used to.
- Constipation: Changes in digestion can show up years before a diagnosis, often dismissed as normal aging or diet related.
- Sleep disturbances: REM sleep behavior disorder, where people act out dreams, can be an early indicator.
- Depression or anxiety: Mood changes may appear without an obvious cause and can precede motor symptoms.
- Fatigue and low motivation: Seniors may feel unusually tired or lose interest in activities they once enjoyed.
- Cognitive slowing or “brain fog”: Subtle changes in memory, attention, or problem-solving can be an early sign.
Because these symptoms are frequently misunderstood or attributed to normal aging, families and caregivers play a key role in noticing patterns and seeking evaluation. Recognizing non-motor signs early allows seniors to get timely support, tailored care, and strategies that make daily life safer and more manageable.
Early Motor Changes in Seniors
After non-motor signs, Parkinson’s in seniors often begins to show subtle motor changes, but these appear gradually, not all at once. Recognizing them early can help families and caregivers support seniors more effectively.
- Smaller handwriting (micrographia): Handwriting may shrink or become cramped over time.
- Shuffling gait: Steps can become shorter and more deliberate, sometimes with a slight dragging of the feet.
- Reduced arm swing: One arm may move less naturally while walking.
- Stiffness or rigidity: Muscles may feel tighter, making everyday movements slower.
- Slower movements (bradykinesia): Tasks that were once quick, like buttoning a shirt, may take longer.
- Difficulty rising from chairs: Standing up may require more effort or a push from the arms.
These changes develop gradually and can easily be mistaken for normal aging. Observing patterns over time, rather than isolated incidents, is key to understanding when a senior may benefit from a professional evaluation or additional support at home.
When Tremors Actually Appear
Tremors are the symptom most people associate with Parkinson’s disease, but they are not always the first sign, and they don’t occur in every senior. Many individuals experience years of non-motor or subtle movement changes before any shaking becomes noticeable.
In some cases, tremors may develop later as the condition progresses. In others, they remain mild or never become a primary symptom at all. Parkinson’s can present differently from person to person, which is why focusing only on shaking can delay recognition of the disease.
Understanding that tremors are just one possible symptom helps families and caregivers pay attention to the broader picture of changes in movement, behavior, and daily function.
Parkinson’s vs. Normal Aging
| Normal Aging | Possible Parkinson’s Disease |
|---|---|
| Occasional stiffness, especially after inactivity | Gradual, ongoing slowing of movement |
| Slightly slower reaction times | Symptoms more noticeable on one side of the body |
| Mild forgetfulness that does not disrupt daily routines | Persistent muscle stiffness that does not improve with activity |
| Movements remain automatic and natural | Loss of automatic movements such as arm swing, facial expression, or blinking |
| Changes tend to stay stable over time | Symptoms are progressive and become more noticeable |
Key takeaway: Normal aging changes are usually mild and stable, while Parkinson’s symptoms tend to progress and worsen over time. Recognizing this pattern helps families seek medical guidance and put supportive measures in place early.
Risk Factors That Increase Parkinson’s Risk in Seniors
While Parkinson’s disease can affect anyone, certain factors may increase the likelihood of developing it later in life. Having one or even several of these does not mean a person will develop Parkinson’s, but awareness can help families stay attentive to early changes.

Common risk factors include:
- Age 60 or older
- A family history of Parkinson’s disease
- Being male
- Long-term environmental exposures, such as certain chemicals or pesticides
- A history of significant head injury
- Specific genetic markers linked to the condition
Understanding risk factors gives caregivers and seniors helpful context. When combined with noticeable symptoms, they can signal that it may be time to seek a professional evaluation or additional support.
When to See a Doctor
Not every change in movement or mood points to Parkinson’s. However, certain patterns suggest it’s time for a professional evaluation. Acting early can bring clarity, rule out other conditions, and open the door to supportive care options.
Consider scheduling a medical appointment if you notice:
- Symptoms that last six months or longer
- Changes that begin to interfere with everyday tasks
- Repeated falls or ongoing balance concerns
- Sleep disturbances that include movement, kicking, or acting out dreams
- Motor changes that are more noticeable on one side of the body
Seeking medical guidance doesn’t mean a diagnosis is certain. It simply ensures that seniors receive appropriate attention, monitoring, and recommendations to maintain safety and quality of life.
How Parkinson’s Is Diagnosed
Diagnosing Parkinson’s disease isn’t about a single lab test or scan, it’s a clinical process that combines careful medical evaluation with the exclusion of other possibilities, as outlined by trusted sources like the Parkinson’s Foundation and the National Institutes of Health (NIH).
A doctor (often a neurologist) will start with a comprehensive neurological evaluation, including a detailed review of the senior’s symptom history and how those symptoms have developed over time. They will observe movement, balance, coordination, and other physical signs to look for patterns consistent with Parkinson’s.
Because there is no definitive “Parkinson’s test,” imaging studies like MRI or dopamine transporter scans (DaTscan) are usually used to rule out other conditions with similar symptoms (such as stroke or structural brain changes), rather than to confirm Parkinson’s itself.
In some cases, doctors may also use lab work or specialized criteria to clarify the diagnosis, but the foundation remains a thorough clinical assessment, putting the person’s symptoms, history, and physical findings together in one picture.
Why Early Recognition Matters
Early awareness gives seniors and families valuable time to plan, adapt, and put supportive strategies in place. Addressing symptoms sooner helps improve safety, preserve independence, and reduce stress for everyone involved.
Establishing structure can also make daily life more manageable. Creating daily routines for seniors living with Parkinson’s can help reduce confusion, support mobility, and maintain confidence at home as symptoms evolve.
The Role of Caregivers and Family Members
Family members and caregivers are often the first to notice when something changes. Because Parkinson’s can begin subtly, the small differences seen day to day such as a slower walk, softer voice, reduced energy, or new sleep issues, may be easiest for loved ones to recognize.
Caregivers play an important role in observing patterns and tracking how symptoms progress over time. Sharing these details with medical providers can make appointments more productive and help doctors understand what a senior is experiencing at home, not just in the exam room.
Support also extends to attending medical visits, helping remember recommendations, and assisting with follow-through once everyone is back home. Even simple steps like organizing medications or reinforcing therapy exercises can make a meaningful difference.
Safety is another major focus. Caregivers frequently help with fall prevention, removing tripping hazards, improving lighting, and offering a steady hand when balance is uncertain. They may also provide daily routine support, ensuring meals are prepared, personal care is completed, and activities remain manageable and stress-free.
Above all, consistent involvement from family and caregivers helps seniors feel supported, understood, and less alone as they navigate changes.
Specialized Parkinson’s Support at Home in Weston, FL
Living with Parkinson’s brings changes, but seniors do not have to face them alone. With the right help, many older adults continue to live safely and comfortably in the homes they love while maintaining routines that bring meaning to each day.
Professional caregivers trained in Parkinson’s support understand how symptoms can affect mobility, balance, energy levels, and daily tasks. They provide steady assistance with personal care, medication reminders, meal preparation, fall prevention, transportation to appointments, and the encouragement seniors need to stay engaged and confident. Just as important, they offer families peace of mind knowing someone experienced is there.
If you’re noticing changes in a loved one or navigating a recent diagnosis, compassionate guidance can be extremely beneficial.
A Place At Home – Weston provides personalized Parkinson’s home care designed to adapt as needs evolve. Whether support is needed for a few hours a week or more comprehensive daily assistance, our care team is ready to help seniors maintain dignity, independence, and quality of life.
Reach out today to learn how specialized in-home Parkinson’s care can support both your loved one and your family in Weston, FL and the surrounding areas. Call (954) 335-9284

Parkinson’s Disease Related FAQs
Can a person have Parkinson’s disease and not have tremors?
Yes. A person can have Parkinson’s disease without ever developing noticeable tremors.
While tremors are the most widely recognized symptom, they are not required for a Parkinson’s diagnosis.
Many seniors experience other symptoms first, such as slowed movement (bradykinesia), muscle stiffness,
balance changes, or non-motor symptoms like sleep disturbances, constipation, depression, or loss of smell.
In some cases, tremors remain mild or never appear at all.
How can you tell the difference between essential tremor and Parkinson’s disease?
Essential tremor usually occurs during movement (such as writing or holding objects),
affects both sides of the body, and does not cause stiffness or slowed movement.
Parkinson’s tremor typically happens at rest, starts on one side, and is often accompanied
by rigidity, slowed movement, and balance changes.
How does Parkinson’s tremor start?
Parkinson’s tremor usually begins gradually and subtly. It most often starts on one side of the body,
commonly in one hand or fingers, and appears while the limb is at rest.
Early Parkinson’s tremor can be intermittent, showing up during periods of stress, fatigue, or anxiety
and disappearing at other times. As the condition progresses, the tremor may become more consistent and
can spread to the other side of the body, though it is not always the most disruptive symptom.