As people live longer, healthier lives, the question of when someone is considered elderly has become less clear. Is it 60? Is it 65? Or does age alone even tell the full story?
Understanding just what defines an age-for seniors, families, and caregivers-can help with planning, decision-making, and conversations about aging and health independence and eventual care needs. The short answer is that both 60 and 65 are in common use, depending on context. The longer answer is more complicated:
Is 60 Considered Elderly?
Yes, in some settings-60 is considered the beginning of older adulthood, but not necessarily “elderly” in the traditional sense.
It is used by, commonly: Age 60
- Central organizations for international health
- Programs for Seniors in the Community
- Social and cultural definitions of aging
Many senior centers, wellness programs, and public health discussions begin using the term older adult or senior at age 60. However, most people at this age are still active, independent, and working or newly retired.
Because of this, age 60 is more accurately described as the start of later adulthood rather than old age.
Is 65 the Start of Old Age?
The age of 65 was quite arbitrary, as this is usually considered the age when one is labeled elderly, primarily because it coincides with retirement, senior benefits, and age-related healthcare planning. However, it is less of a rule and more of an outline than an actual measure of health or competency. The majority of people at age 65 live active, independent, and productive lives.
This is largely because age 65 marks eligibility for major milestones such as:
- Medicare health insurance
- Certain retirement and senior benefits
- Age-based healthcare screenings
For decades, age 65 has been used as a benchmark in healthcare, policy, and retirement planning. As a result, it has become the most widely accepted definition of when someone is considered elderly—at least administratively.
Still, many adults at 65 remain healthy, active, and fully independent.
Why There’s No Single Definition of “Elderly”
There is no definition of the word elderly, since aging is a different process for each person.
Chronological age, or the age a person is, does not always reflect:
- Physical ability
- Cognitive health
- Emotional well-being
- Independence in daily life
Two persons aged 70 years may have very different health profiles and support needs. That is why many professionals today focus less on age alone and more on functional aging.
What is Functional Age and Why Should It Matter?
Functional age describes how well a person functions in daily life, other than how old they are by years. It is a reflection of factors such as one’s mobility and balance, the ability to manage activities of everyday living, memory and decision-making, and overall health and stamina. From a care perspective, functional age often means more than chronological age. Whereas some people in their late 70s are still fully independent, some others in their early 60s may require daily support as a result of illness, injury, or health changes.
Does turning 60 or 65 mean a person needs care?
No–an increase in years does not make any person pop into the care category. Many adults remain independent, living in their communities well into their 80s and beyond. The basis for most care decisions includes:
- Safety at home
- Ability to perform daily activities
- Health changes
- Recovery after surgery or illness
- Level of family support
Age may be a reference point, but care needs are driven by function and safety, not a number.
At What Age Qualifies Seniors for Federal Programs and Senior Benefits?
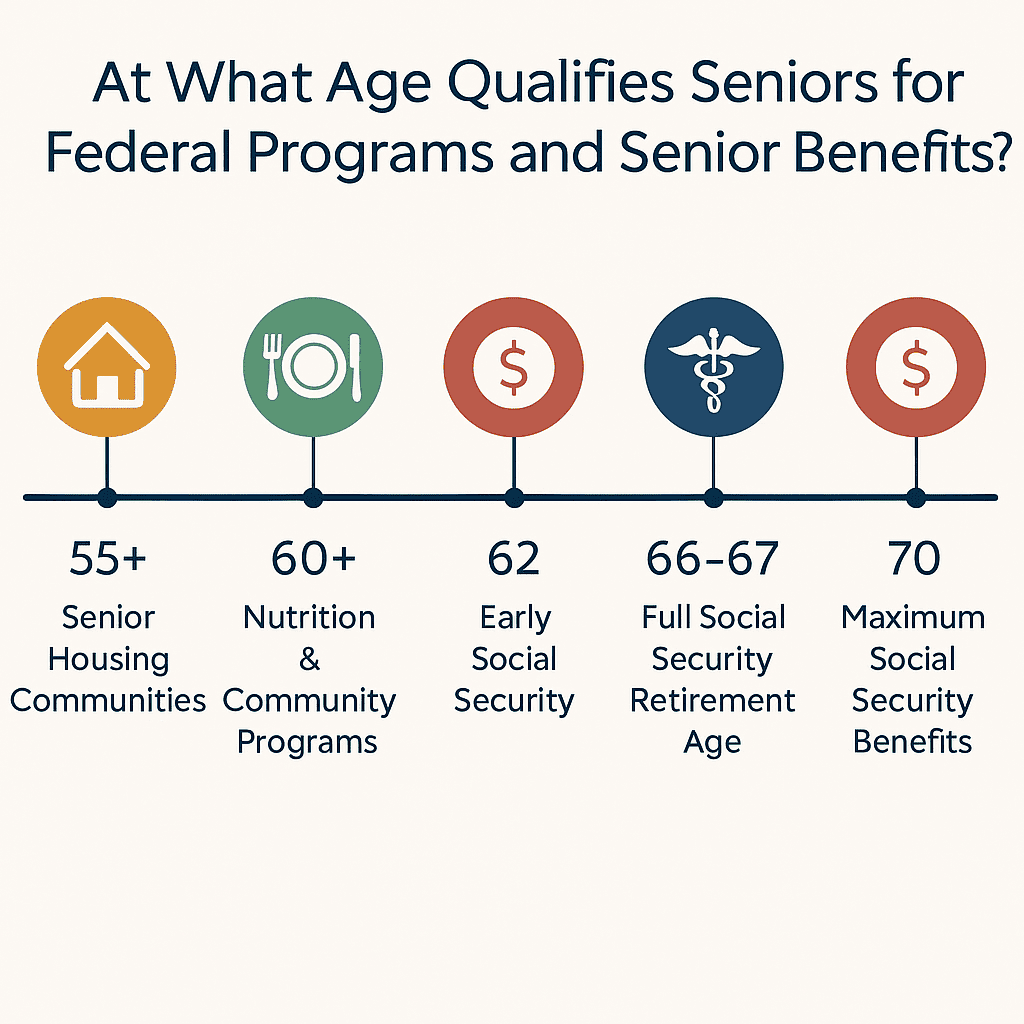
Most of the senior benefits are attached to an age threshold instead of a single definition of “elderly” in the United States. These programs are made for healthcare access, income security, housing, and daily living as one is aging. The most widely applied benchmark is 65, although under or over this level of age, eligibility can begin for different programs.
Medicare (Age 65)
Attains Medicare eligibility at an elderly stage of life, which begins at 65 years, providing them with health insurance. The programs offered under Medicare cover hospital and medical treatment and prescription drugs. Attaining Medicare is one of the reasons why a person attains senior status when they reach 65 years.
Social Security Retirement Benefits (Ages 62–70)
Benefits for retirement under Social Security can be drawn from as early as 62 years of age, but they are reduced if one wishes to start taking them before attaining full retirement age. Benefits are available from 66 to 67 years of age, with an option to raise them if one delays taking them until 70 years of age.
Supplemental Security Income (SSI) (Age 65 or Disability-Based)
SSI offers financial assistance to senior citizens with limited income and resources. Although eligibility can start at 65, some people can become eligible before this time if they have a disability. Assistance from this social service will cover basic living needs such as food and shelter.
Medicaid and Long-Term Care Assistance (Varies by State)
Eligibility for Medicaid benefits is determined by income and resources, but not by age, and many people can become eligible when their care requirements escalate in old age. Medicaid benefits include assistance with long-term healthcare such as in-home and SNF care.
Housing Assistance and Senior Housing Programs (Age 55+ or 62+)
Numerous government and local programs exist for senior citizens beginning at either age 55 or 62 years. Such programs can include rent subsidies, senior-only apartment buildings, and senior-friendly living communities.
Benefits for Veterans Aged 65 and Older (Varies by Benefit)
Veterans may be eligible for healthcare benefits, pensions, and assistance programs when they reach advanced age. Benefits come with eligibility based on age, military service, financial need, or disability.
Nutrition and Community Support Programs (Often Age 60+)
Programs such as congregate meal services, home-delivered meals, and senior community services often begin at age 60. These services support nutrition, social engagement, and independent living for older adults.
Apart from benefits and eligibility, other dimensions of life in which aging might be considered include phases of life in order to address varying requirements at different stages.
Is “Senior” the Same as “Elderly”?
Often, people will use these terms interchangeably, but “older adult” or “senior” can be a better option because it sounds more respectful and less concentrated on vulnerability. “Elderly” may be a common term in a medical or a government setting, but usage is moving toward someone-first languages.
Although it does not in itself define aging or need, age is a factor in establishing eligibility for two very important government programs.

What are the Stages of Aging?
Aging can be described in terms of phases in order to have a better understanding of health, autonomy, and function. Although different authors describe phases in different ways, a generally accepted model consists of four phases:
- Early Older Adulthood (commonly 50s to early 60s): Here, people are active and self-sufficient but may have to deal with chronic ailments or lifestyles.
- Young-old (commonly 65-74 years old): Generally, it involves transitions into retirement, a heightened emphasis on preventive health care, maintaining mobility, and autonomy.
- Middle-old (often 75–84): Some adults may need assistance occasionally with transportation, household chores, taking medications, or personal safety at home.
- Old-old (85+): Needs for assistance are more likely to increase, especially with fall risk, memory changes, and help with activities of daily living.
These stages aren’t strict rules. They’re a helpful way to talk about aging in a realistic, respectful way—because people age differently based on health, environment, and support systems.
At What Age Do Seniors Commonly Begin Requiring Assistance?
There is no specific age at which someone suddenly needs care. Most support needs develop gradually and are driven by functional changes, not birthdays. Challenges such as loss of mobility, balance problems, forgetfulness, managing daily activities, taking medications, or safety in and around the dwelling are more likely considerations before support is actually required. Some people can continue to look after themselves well into their 80s, where others will require support in their early 60s.
When Should Families Start Planning for Senior Care?
The best time to plan for senior care is before a crisis occurs. Families often benefit from starting conversations and exploring options once a loved one begins experiencing falls, trouble managing medications, difficulty cooking or keeping up with household tasks, or needs extra support after a hospital stay. Early planning allows families to make thoughtful, less stressful decisions and put the right support in place before safety or health becomes urgent.
Is the Term “Elderly” Still Appropriate?
The word elderly is increasingly being replaced with terms like:
- Older adult
- Senior
- Aging adult
This shift reflects a more respectful and accurate view of aging. Many people associate “elderly” with frailty, which does not represent most adults in their 60s or even 70s.
Using people-first language helps focus on ability, not limitation.
Senior Home Care from A Place At Home – Summerlin
Every individual grows old in a different way, and when they need help, it is not based on a certain age. The most important factor is safety, independence, and a good life at home. A Place At Home – Summerlin residents will have access to tailor-made senior home care, which will address each individual in a manner in which they can be assisted either occasionally or on a continual basis.
Our caregivers assist senior citizens in being comfortable and self-reliant in their homes by providing assistance with personal care, meal service, medication reminders, mobility support, friendship, and post-illness recuperation. We assist the family in adjusting this support based on their evolving requirements, keeping in mind their dignity and continuity of care.
If you are just starting to think about planning for the future or if you notice some signs that a loved one in your life may need a little extra assistance, our local team is available to walk you through this next step.
Final Takeaway
Whether a person can be labeled as senior at 60 or at 65 can very much depend on the context in which they are being assessed. The truth is, aging is far more a function of health, independence, and functionality relative to a number.


