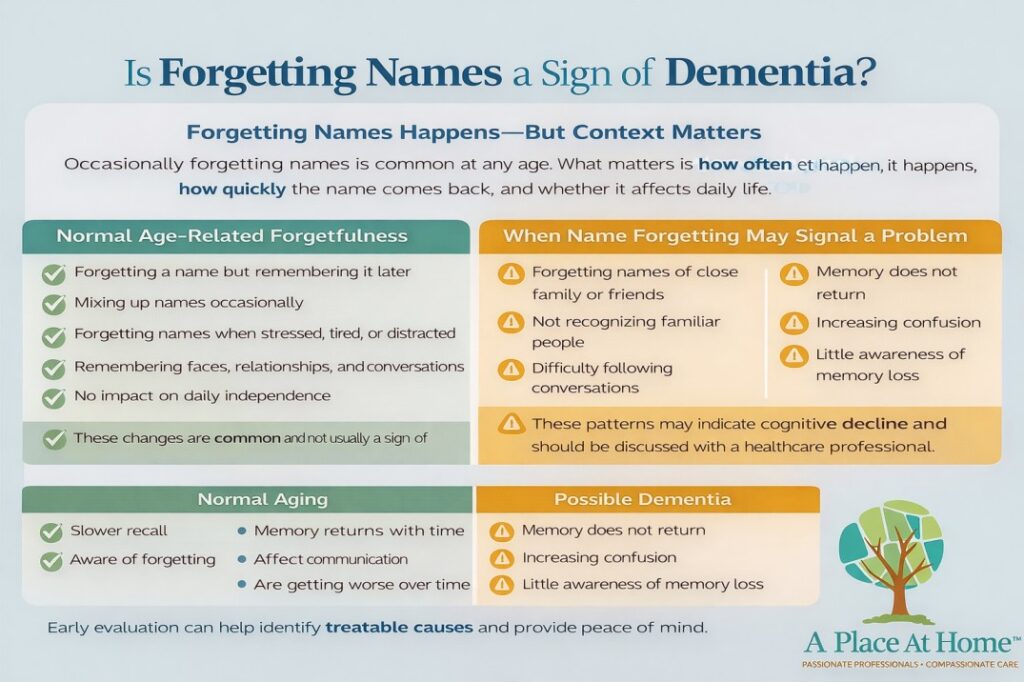
Forgetting names is a common experience for seniors and aging adults, and occasional lapses are usually a average part of aging. However, if your parent or loved one frequently forgets names, repeats questions about familiar people, or shows waning memory over time, it could be an early sign of dementia. Caregivers and families should pay attention to patterns of memory loss, as recognizing changes early can help provide timely support, in-home senior care, and strategies to maintain independence for aging adults.
Understanding memory and the aging brain
Memory is a complicated process that involves determining, storing, and saving information. As adults age, it is natural for some cognitive changes to occur:
- Slower recall: Names and details may take longer to remember.
- Occasional lapses: Forgetting items, forgetting appointments, or struggling to recall names temporarily is common.
- Distracted memory: Busy schedules or stress can make it harder to remember details, including people’s names.
These experiences are normally mild and do not affect daily life, but understanding the difference between normal forgetfulness and signs of dementia is key for families and older adults alike.
Why seniors forget names
Forgetting names is a common experience for seniors and older adults, and it is usually a normal part of aging. Names are often harder to remember because they are arbitrary labels with no inherent meaning, making them more difficult for the brain to store and memory. Additionally, seniors may use certain names infrequently, so the lack of repetition can make recall even harder. Everyday stress, distractions, or multitasking can also affect memory, as the brain battles to focus on and retain information. Finally, normal intellectual slowing that occurs with age means the brain procedures information more slowly, which can make retrieving names feel more challenging. While these factors are typical for aging adults, repeated or persistent struggles may signal the need for further evaluation.
Signs that forgetting names may indicate dementia
For seniors and aging parents, it’s important to differentiate normal memory lapses from early signs of dementia. Warning signs include:
- Forgetting names of close friends or family members frequently
- Memory problems that interfere with daily routines, such as missing appointments or repeating conversations
- Difficulty recalling recent events or discussions
- Misunderstanding in familiar settings, like getting lost in a neighborhood they know well
- Trouble finding the right words or completing conversations
- Changes in mood or personality, including increased anxiety, irritability, or social withdrawal
Persistent memory loss that influences daily life is often an early symptom of dementia and warrants a medical evaluation.
How can you tell if a senior is showing early signs of dementia?
Telling if a senior is showing early signs of dementia needs careful observation and practical assessment in everyday life. Instead of just observing memory lapses, you can use real-life approaches to see if cognitive changes are continuing and impactful.
Ways to tell if a senior may have early dementia:
- Observe daily activities: Watch how they handle routine tasks like cooking, managing medications, paying bills, or following simple instructions. Difficulty completing these tasks can indicate cognitive decline.
- Track memory patterns: Keep a journal of what the senior forgets, how often, and in what situations. Frequent, repeated forgetfulness—especially about names, appointments, or recent events—is more concerning than occasional lapses.
- Test orientation subtly: Ask questions about the day, date, or location during casual conversation. Confusion that appears repeatedly may signal early cognitive changes.
- Notice communication changes: Involve them in conversation and observe if they struggle to find words, substitute incorrect words, or have trouble following discussions.
- Monitor judgment and decision-making: Watch for unusual or risky decisions, such as mismanaging money, ignoring safety, or forgetting personal hygiene.
- Watch social behavior: Notice if they start withdrawing from interests, friends, or activities they once enjoyed, or if mood changes suddenly without clear cause.
The key is constant observation over time. One or two isolated incidents are usually normal aging, but persistent patterns in multiple areas should prompt a professional evaluation.
Factors that can mimic dementia
Not every memory problem in older adults is caused by dementia. Other factors can temporarily affect memory, including:
- Stress or anxiety, which can interfere with attention and recall
- Sleep deprivation, which impairs brain function and consolidation of memories
- Medication side effects that cause confusion or forgetfulness
- Vitamin deficiencies, particularly vitamin B12, which can impact cognitive function
- Depression or mood disorders, which often mimic memory decline in seniors
Addressing these factors can improve memory without the need for dementia-specific interventions.
How Families Can Help Seniors Who Often Forget Names
Frequent forgetfulness, especially when it comes to names, can be concerning for both seniors and their families. Taking early, proactive steps can help your loved one maintain independence and support their cognitive health. One of the first things families can do is keep a memory log, recording when forgetfulness occurs, any patterns, and how often it happens. This record becomes an important tool for doctors to understand whether memory lapses are occasional or part of a larger cognitive issue.
It’s also important to observe how memory challenges affect daily life. Forgetting names can impact routines, safety, and social interactions, making it clear whether additional support is needed. Seeking a professional evaluation is a crucial next step. A healthcare provider can assess overall cognitive function and rule out treatable causes of memory loss, such as medication side effects, vitamin deficiencies, or sleep problems.
Doctors may recommend formal cognitive testing, including exams like the Mini-Mental State Exam (MMSE) or the Montreal Cognitive Assessment (MoCA), to detect early changes and provide a baseline for monitoring. Beyond professional evaluation, families can encourage brain-healthy habits that support memory. Regular physical activity improves blood flow to the brain, while a balanced diet rich in fruits, vegetables, and healthy fats supports cognitive function. Social engagement, including conversations with friends or family and participation in community activities, keeps the mind active and connected. Mentally stimulating activities, such as reading, puzzles, or learning new skills, can further reinforce memory and focus.
How a Home Caregiver Can Help When Memory Changes Appear
As seniors experience memory changes, even mild forgetfulness can make daily routines more challenging and affect their independence. This is where a trained home caregiver from A Place at Home – Summerlin, NV can make a real difference. Caregivers provide support with daily tasks, companionship, and safety monitoring, helping seniors continue to live comfortably at home.
A home caregiver can assist with:
- Managing daily activities, like cooking, bathing, medication reminders, and housekeeping
- Ensuring safety, such as preventing accidents, helping seniors navigate their environment, and keeping routines consistent
- Providing companionship and mental engagement, reducing feelings of isolation and supporting cognitive health
- Observing changes in memory or behavior, so families can notice patterns early and respond appropriately
With in-home care, seniors can maintain their independence, feel secure, and enjoy personalized support tailored to their needs, while families have peace of mind knowing their loved ones are cared for.
Also Read: How Long Can Someone Live with Dementia?