When a loved one with dementia can no longer communicate verbally, family members face one of the hardest times in their lives. People start to think “How long will this person live?” or “What can I do to keep this person comfortable?” The answer is different for each individual; by understanding dementia at this stage, you can help provide care that maintains dignity, compassion and patience.
What Does “Nonverbal” Mean in Dementia?
Dementia patients who lose the ability to speak indicate late stages of dementia. The brain areas responsible for speech and language will be affected, causing difficulty or inability for the patient to be able to speak.
But nonverbal does not mean unaware. Many patients will still have a sense of tone, emotion and facial gestures, so they will find a way to communicate with you—through smiles, hand-clasping, or eye contact—without using words. Family members will be able to learn more about the other ways patients can connect through forms of communication that remain open and available.
What Are the Common Signs of Late-Stage Dementia?
Even when your loved one can no longer speak, they are still communicating in their own ways, and subtle changes in their abilities can help guide the care they need. Some of the most common signs families may notice include:
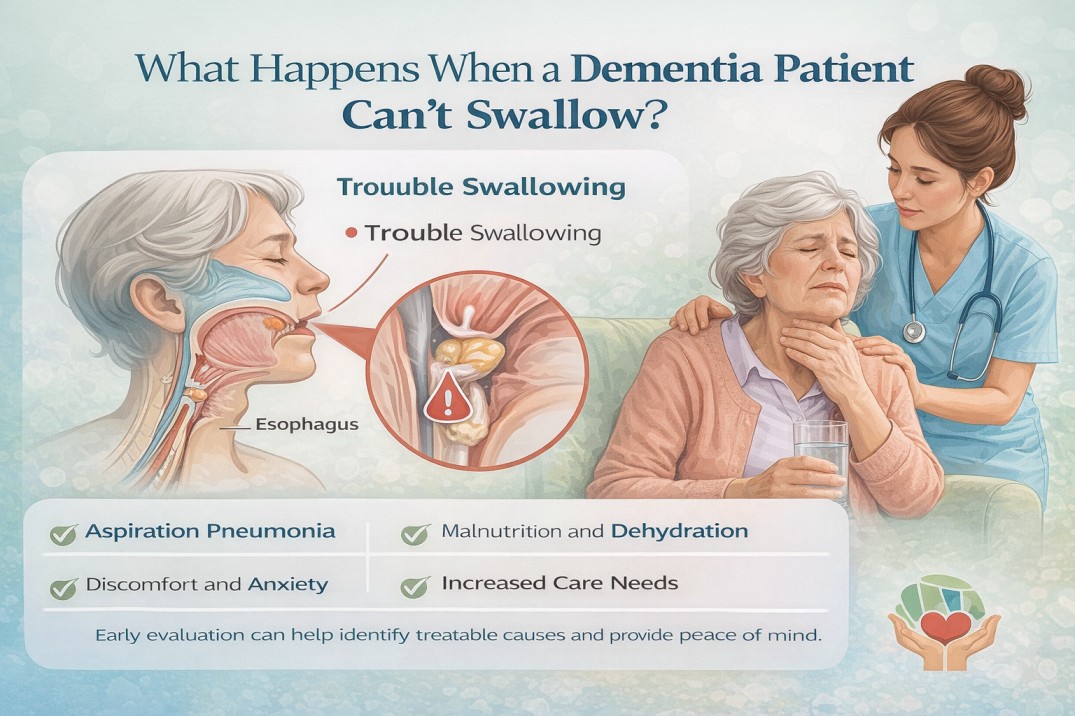
- Eating and swallowing difficulties: Meals may become challenging, and your loved one might need gentle guidance or assistance to stay nourished.
- Reduced mobility or independence: Tasks they once managed easily may now require support, reminding you of their growing vulnerability.
- Changes in sleep and activity patterns: They may sleep more during the day or become restless at night, signaling shifts in comfort and energy.
- Subtle reactions to touch, music, or familiar voices: Even without words, familiar sounds and gestures can spark recognition, calm, or joy.
Paying attention to these signs allows families to plan care thoughtfully, respond before small issues become emergencies, and most importantly, ensure that your loved one continues to feel seen, safe, and loved.
How Long Do Nonverbal Dementia Patients Typically Live?
Life expectancy during this time period will vary greatly between individuals due to various factors including but not limited to: Type of dementia (Alzheimer’s, Vascular, Lewy body etc.), Health history and any associated medical problems; Nutrition, Mobility, Ability to swallow safely. Additionally, Complications such as Infections may also play a part in determining how soon a person declines.
According to research and experiences of Caregivers, vis-à-vis, the word “nonverbal”, it is estimated that many people suffering from Dementia begin experiencing a marginal rate of survivability between several months and a few years after reaching the point of Non-Verbal communication. The average estimates from several studies indicates that most people who suffer from Dementia have a life expectancy of between 6 months and 2 years after reaching the non-verbal stage. However, this is only an estimate and there are exceptions to this general rule – specifically some individuals will have longer life expectancy rates depending upon regular quality of Care and support, whereas others will experience quickened rates of decline based on differing circumstances.
How to Care for a Nonverbal Dementia Patient
Even when your loved one can no longer speak, connection is still possible. There are many ways to communicate and show love that go beyond words:
- Be present and use gentle touch: Holding hands, softly stroking their arms, or simply sitting close can provide reassurance and a sense of safety.
- Speak with tone and expression: Even if they can’t respond verbally, a calm, warm voice conveys comfort, love, and stability.
- Maintain routines: Consistent meals, rest, and familiar activities help reduce anxiety and give structure to their day.
- Engage the senses: Music, pleasant scents, or soft textures can evoke memories and emotions, helping your loved one feel more connected to the world around them.
- Support nutrition and hydration: Adaptive feeding methods, smaller bites, or consulting a speech therapist can make eating safer and more comfortable.
These small, thoughtful efforts may seem simple, but they have a profound impact. They help your loved one feel seen, safe, and loved, maintaining connection even when words are no longer possible.
Activities Even for Nonverbal Patients
Even without speech, your loved one can enjoy meaningful activities:
- Listening to music, singing together, or humming along
- Gentle stretching or guided movement exercises
- Reading aloud, storytelling, or looking through photo albums
- Sensory stimulation using soft fabrics, scented objects, or nature sounds
These activities promote emotional engagement and reinforce connection, showing that love and communication go beyond words.
Conclusion
Caring for a nonverbal dementia patient is challenging, but it’s also an opportunity to connect in ways that go beyond words. Gentle touch, familiar routines, music, and thoughtful observation can help your loved one feel safe, loved, and understood—even in late-stage dementia.
Many families find that having additional support at home can make a big difference. A compassionate home care companion in Kirkland, for example, can spend a few hours a day engaging your loved one, assisting with meals, and providing comfort, while giving family caregivers much-needed relief. Combining this support with attentive daily care ensures your loved one maintains dignity, comfort, and meaningful connection throughout this stage of life.
Remember, even small acts of presence, patience, and love can profoundly impact your loved one’s quality of life.