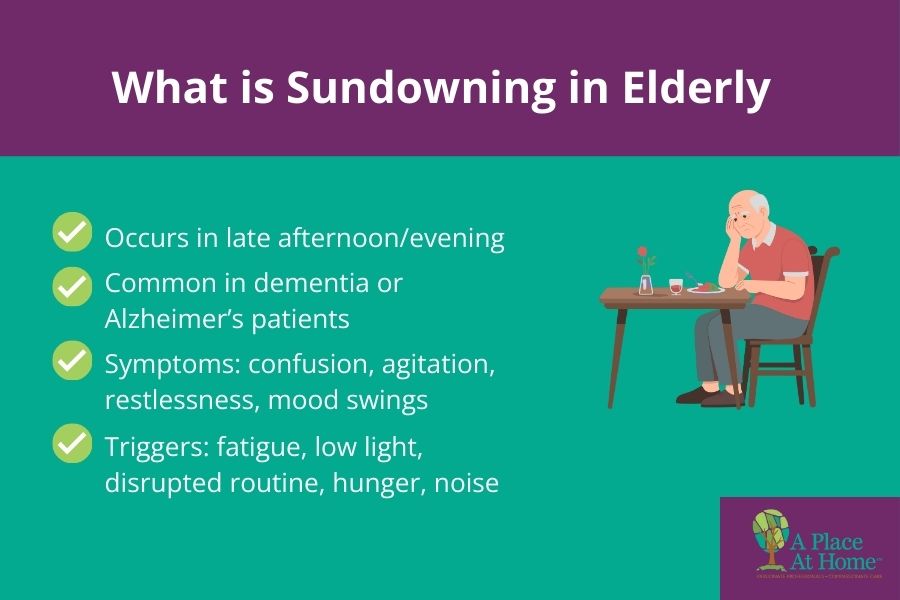
Seniors who become confused or agitated at night may be experiencing sundowning syndrome, a common symptom associated with dementia. This condition can trigger a range of behaviors, including anxiety, disorientation, and restlessness. Understanding why sundowning occurs helps caregivers provide better support and comfort to their elderly loved ones.
Alzheimer’s disease and other forms of dementia cause cognitive changes that can lead to sundowning, also referred to as sundowning syndrome. While the exact cause is not fully understood, sundowning is not a disease itself but rather a recognizable pattern of symptoms that often appears in the late afternoon or evening.
What Is the Difference Between Nighttime Confusion and Sundowning?
Nighttime confusion broadly refers to disorientation, agitation, or restlessness that appears after dark. Sundowning is a dementia-related form of nighttime confusion where symptoms worsen specifically in the late afternoon or evening.
A simple distinction:
- Nighttime confusion = the symptom
- Sundowning = dementia-related cause of those symptoms
What are symptoms of sundowning?
Confusion and anxiety can arise in older adults diagnosed with dementia when the sun sets. In addition to acting confused, they may cry, pace, rock in their chair, or hallucinate. Trouble distinguished dreams from reality is another common symptom of sundowning.
Aging people experiencing sundowning may shadow their caregiver (follow them around wherever they go). Wandering, difficulty sleeping, and yelling are also symptoms. As the sun dips below the horizon, the dementia patient may even lash out violently at caregivers and other individuals.
What Time Does Sundowning Usually Start?
Most families notice symptoms beginning in the late afternoon or early evening, typically between 4 p.m. and 8 p.m. As outdoor light fades, fatigue increases and the environment becomes quieter, which can intensify confusion.
Can Nighttime Confusion Happen Without Dementia?
Yes. While sundowning is strongly linked to dementia, seniors without dementia may also become confused at night due to:
- Medication side effects
- Sleep apnea
- Dehydration
- Infections such as UTIs
- Hospital environments
- Anxiety or loneliness
- Vision changes after dark
If you’re unsure whether these changes reflect normal memory loss or a form of dementia, this guide on the differences between memory care and dementia care offers clear explanations and signs to look for: Memory Care vs. Dementia Care
What triggers confusion in the elderly?
As mentioned, the cause of sundowning is unknown. However, experts believe the symptoms worsen when seniors are sleep deprived. Older adults need less sleep, but poor sleep quality contributes to sundowning. Dreaming during sleep can disorient them, causing confusion between dreams and reality.
Dementia affects the brain’s internal clock, disrupting their circadian rhythm and causing them to confuse day and night. Nighttime shadows and low light can strike fear and confusion in the elderly and increase their confusion. Sleep apnea, a condition that reduces oxygen, is also a culprit.
Confusion may arise when the older adult navigates or sleeps in an unfamiliar place, such as a hospital. If the senior is bored or lonely, the lack of stimulation can worsen symptoms. Urinary tract infections (UTIs) and other underlying health conditions also create confusion in aging people.
A senior who is hungry, tired or has other unmet needs may respond with confusion at night. Similarly, confusion can develop when the older adult needs to use the toilet and, due to dementia, they forget where the bathroom is located or are unable to process their urge to urinate.
Some medications, like sedatives, also create confusion in seniors. This is due to side effects or the drug wearing off closer to bedtime. Certain statins prescribed to control cholesterol levels as well as common heart medications disrupt sleep and cognitive function, leading to confusion and delirium.
Dehydration is a known but easily overlooked contributor to confusion in elderly individuals. Due to naturally decreased thirst sensations, older people may not recognize that they are thirsty and become dehydrated. Or mobility challenges can interfere with their access to daily fluids.
How Long Does Nighttime Confusion Last?
Episodes may last anywhere from a few minutes to several hours. In dementia, sundowning may happen some evenings but not others. Consistency in routine, lighting, and sleep patterns can reduce the duration.
When Should Families Call a Doctor?
Contact a healthcare provider if nighttime confusion:
- Appears suddenly
- Worsens quickly
- Includes fever, pain, or hallucinations
- Causes aggressive or unsafe behavior
- Prevents the senior from eating, drinking, or sleeping
How do caregivers lessen seniors’ confusion at night?
1. Avoid Caffeine
Confusion and other effects of sundowning can be mitigated with the right support. Caregivers help their elderly care recipients reduce symptoms by not serving caffeinated beverages after morning. Caffeine disrupts sleep, overstimulates the aging brain, and prevents seniors from relaxing.
2. Ensure Hydration
Hydration is critical to maintaining brain function and preventing confusion. Dehydration, conversely, worsens cognitive health and leads to increased confusion, especially at night when the elderly drink less fluids. Ensure the senior remains hydrated to support clear thinking and combat confusion at night.
3. Stick to Routine
Establish a schedule with regular times for waking up, eating meals and going to bed. A predictable routine reduces anxiety and signals to the body when to wind down. Daily structure offers the older adult comfort, security, and minimizes disorientation in the dark.
4. Arrange Daytime Activities
A senior with dementia is more alert during the day. Caregivers should schedule doctors’ appointments and activities in the morning hours to leverage dementia patients’ increased alertness. While at the physician’s office, ask about the best times of day for the senior to take medications.
5. Spend Time Outdoors
Caregivers can further reduce the elderly care recipient’s restlessness by taking leisurely walks outdoors. Sunlight is beneficial as it provides clear day and night cues, thereby reducing the senior’s disorientation and other sundowning symptoms. It also promotes daytime alertness and nighttime sleep.
6. Increase Indoor Lighting
Since nighttime shadows provoke confusion in seniors with dementia, keep the home well-lit in the evening. Identify and pursue calming activities with the older adult, like flipping through a family photo album, watching a beloved movie, or listening to soothing music.
7. Promote Nighttime Rest
If sleeping restfully at night is difficult, limit the senior’s daytime naps. In the evenings, create a relaxing environment to promote sleep. Reduce stimulations, such as loud music, television and screen time, which can distract the elderly person and create more confusion.

Overnight Care from A Place At Home
Nighttime can spur confusion in seniors with dementia. Reduce their symptoms with the help of compassionate caregivers from A Place At Home. Our reputable home care agency supports the unique needs of the elderly with a comprehensive range of non-medical in-home care services.
Families may prefer overnight care, where providers assist the senior with bedtime tasks. We help with personal hygiene, including toileting and dressing for bed. Our overnight caregivers are ready to provide mobility support when the senior needs to use the bathroom at night.
Arrangements may be made so overnight caregivers sleep in the same room with the older adult or occupy a nearby space with quick access to the senior. Caregivers are also trained to respond appropriately and swiftly to emergencies or urgent needs that develop at night.
Overnight care is the solution for seniors with dementia who experience confusion. Care options are flexible and can be scheduled for a few nights per week or regularly depending on needs. Older people with vision impairment or who’ve returned from a hospital stay also benefit from our services.
A Place At Home is dedicated to providing dependable senior home care to older adults living in Carrollton, Texas. If the senior in your life needs support to achieve a quality night’s rest, we can help. Schedule a free in-home consultation today to learn more about our highly rated services.
FAQs
How Is Nighttime Confusion Treated?
While sundowning cannot be cured, symptoms can be significantly reduced with the right strategies. Treatment usually involves:
- Adjusting medications (under physician guidance)
- Treating underlying conditions like UTIs or sleep apnea
- Improving sleep habits
- Increasing daytime stimulation
- Caregiver support during high-risk evening hours
Does nighttime confusion get worse in the winter?
Yes. Shorter days, earlier sunsets, and less natural light during winter months can intensify sundowning symptoms. Many families notice more confusion, agitation, and restlessness in the late fall and winter.
Can too many daytime naps cause nighttime confusion?
Excessive or late-afternoon naps can disrupt a senior’s sleep cycle and contribute to restlessness or confusion in the evening. Short, early naps are usually better tolerated.
Can certain foods make nighttime confusion worse?
Sugary snacks, heavy meals, and caffeinated beverages especially in the afternoon may overstimulate seniors, cause indigestion, or interfere with sleep, contributing to confusion at night.
Does watching TV before bed increase confusion for seniors?
Yes. Fast-paced visuals, loud sounds, and screen light can overstimulate the brain, making it harder for seniors with dementia to wind down. Calming music or quiet conversation is a better alternative.
Can nighttime confusion lead to wandering?
Yes. Disorientation and restlessness in the evening can cause seniors to walk aimlessly or attempt to leave the home. This is why close supervision and secured environments are important during sundowning periods.